Sleep apnea is a common yet widely overlooked health condition in Nepal. Many people dismiss symptoms like loud snoring, daytime fatigue, poor focus, or frequent nighttime awakenings as stress or lifestyle issues—when in reality, these may indicate a serious sleep-related breathing disorder affecting oxygen levels and long-term health.
This guide offers Nepal’s most complete and easy-to-understand overview of sleep apnea testing. You will learn about the symptoms to watch for, the different types of sleep tests available, how home sleep tests compare to full overnight studies, the cost of testing in Nepal (including Kathmandu), how accurate these tests are, and what happens before and after diagnosis.
Whether you're considering your first sleep test or exploring treatment options after a diagnosis, this comprehensive resource will help you understand every step clearly and confidently.
CHAPTER 1 Understanding Sleep Apnea
Sleep apnea is a sleep-related breathing disorder in which a person repeatedly stops breathing or breathes very shallowly during sleep. These pauses can last from a few seconds to more than a minute, and may happen dozens—or even hundreds—of times per night.
Because these breathing disruptions occur while a person is asleep, most people don’t realize they have sleep apnea. Often, a family member or partner notices the symptoms first, such as loud snoring, gasping, or long silences between breaths.
1.1 How Sleep Apnea Disrupts the Body
Every time breathing stops:
Oxygen levels drop (oxygen desaturation)
Your blood oxygen saturation (SpO₂) falls, forcing the brain to wake you repeatedly to restart breathing.
The heart works harder
Low oxygen triggers sudden spikes in heart rate and blood pressure. Over time, this increases the risk of:
- Hypertension
- Irregular heartbeat
- Heart failure
- Stroke
The brain is repeatedly interrupted
Even though you might not fully awaken, your sleep cycles are constantly disturbed, preventing restorative deep sleep.
Metabolism becomes imbalanced
Chronic sleep apnea is linked to:
- Weight gain
- Diabetes
- Hormonal imbalances
- Increased appetite (especially late-night cravings)
This creates a cycle where apnea worsens weight, and weight worsens apnea.
1.2 Why Most People Never Realize They Have Sleep Apnea
Sleep apnea is often called a “silent nighttime disorder” because:
- Breathing pauses happen during sleep
- Most awakenings are extremely brief
- Symptoms like fatigue or headaches are dismissed as stress
- Snoring is considered normal in many Nepali households
- Patients rarely connect nighttime snoring with daytime health issues
People can suffer for years without knowing the root cause.
1.3 Types of Sleep Apnea (Simple & Clear)
- Obstructive Sleep Apnea (OSA): The airway collapses or becomes blocked during sleep.
- Central Sleep Apnea (CSA): The brain temporarily stops sending breathing signals.
- Mixed/Complex Sleep Apnea: A combination of obstructive and central events.
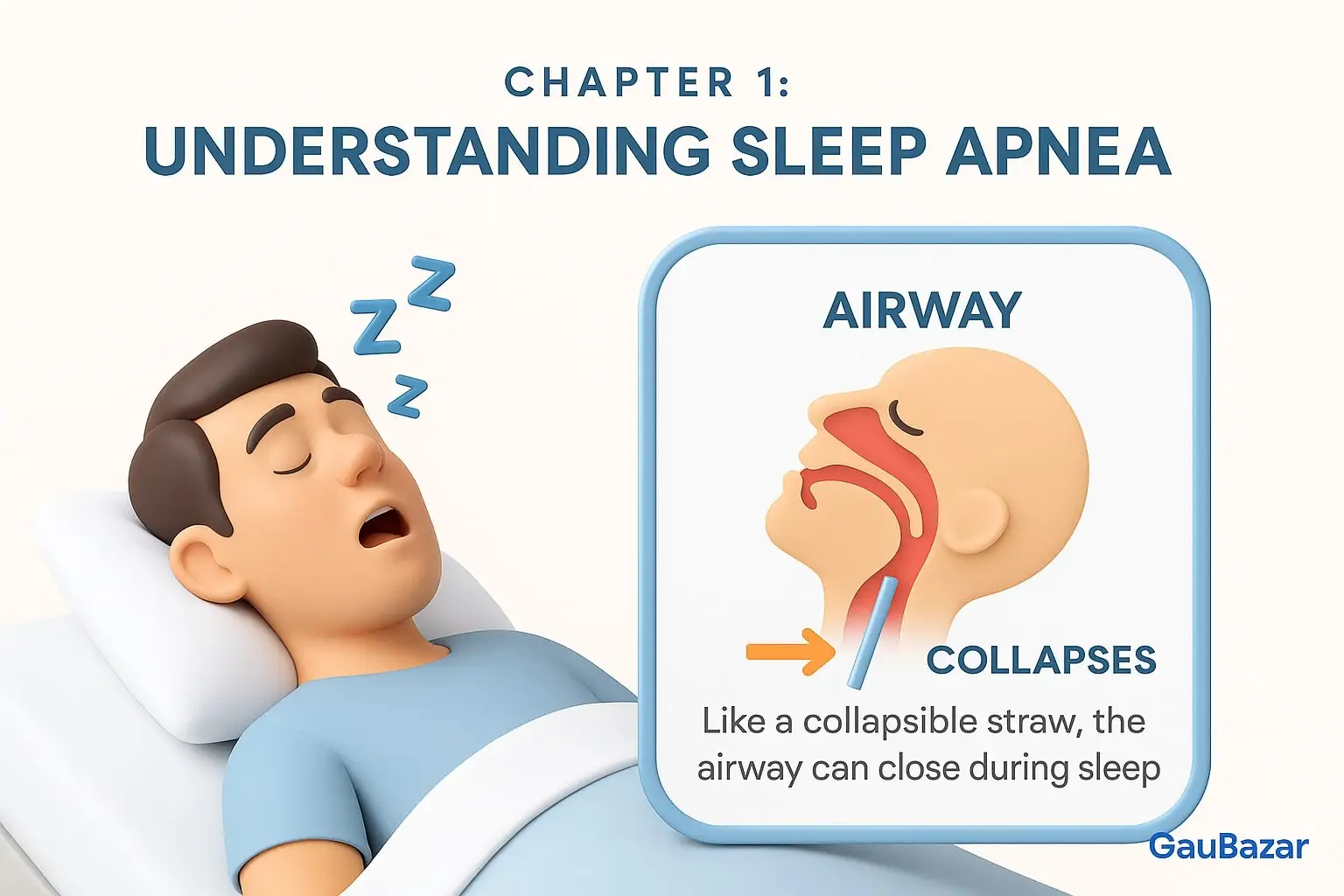
1.4 A Simple Analogy to Understand Sleep Apnea
Think of your airway like a flexible drinking straw.
- When you breathe normally, the straw stays open.
- When you relax during sleep, the straw becomes soft.
- If it collapses, air cannot flow — this is sleep apnea.
- Your brain senses the lack of air and “kicks” you awake to reopen it.
This cycle repeats all night, preventing deep, restorative sleep.
1.5 What Happens During an Apnea Event
Here’s what a single apnea moment looks like:
- Airway collapses → breathing stops
- Oxygen drops → your body panics
- Brain sends a “wake-up signal”
- You take a gasp or snort
- You fall back asleep, unaware of what happened
- Cycle repeats all night
Someone with severe sleep apnea can experience 30–100+ events per hour, meaning the brain never gets proper rest.
1.6 Why Testing Is Important
Sleep apnea cannot be diagnosed based on symptoms alone.
A sleep test is the only way to measure:
- Number of apnea events
- Duration of breathing pauses
- Oxygen levels
- Heart rhythm changes
- Sleep stages (in full PSG)
Accurate diagnosis = proper treatment.
CHAPTER 2 Symptoms Commonly Seen in Nepali Patients
Sleep apnea symptoms often appear gradually, which is why many Nepali patients overlook them for years. Unlike common sleep disturbances, sleep apnea symptoms follow a predictable pattern linked to disrupted breathing and poor oxygen flow during sleep. Recognizing these signs early can prevent serious health complications.
This chapter explains the symptoms clearly—without repeating anything from Chapter 1, and without overlapping content from later diagnostic chapters.

2.1 Nighttime Symptoms (During Sleep)
These symptoms happen while the person is sleeping, often unnoticed by the patient but observed by family members.
Loud, Persistent Snoring
Not all snoring is sleep apnea, but snoring that is:
- Loud
- Frequent
- Continuous
- Worsening over time
…is one of the strongest warning signs. In many Nepali households, snoring is jokingly accepted as normal, causing the disorder to remain undiagnosed.
Pauses in Breathing
Family members often notice long gaps in breathing. These may look like:
- The person “holding their breath”
- Long silence followed by a gasp
- Sudden snorting or choking sound
This is the primary indicator of sleep apnea.
Gasping, Choking, or Snorting
These reflexes occur when oxygen levels drop and the brain pushes the body to breathe again. They often wake up the partner but not the patient.
Restless or Fragmented Sleep
The person may constantly:
- Toss and turn
- Change sleep positions
- Pull blankets
- Wake up briefly without remembering
This happens because the body struggles to maintain normal breathing.
Dry Mouth or Sore Throat Upon Waking
Because people with sleep apnea often breathe through their mouth at night, they wake up with uncomfortable dryness.
2.2 Daytime Symptoms (During Wakefulness)
Daytime symptoms come from poor-quality sleep and low oxygen levels. These often impact personal life, work performance, and long-term health.
Excessive Daytime Sleepiness
People may feel tired even after sleeping 7–8 hours. Common signs include:
- Falling asleep while reading or watching TV
- Struggling to stay awake during meetings
- Feeling sleepy while driving (dangerous in Nepal’s road conditions)
Difficulty Concentrating
Poor oxygen and fragmented sleep affect brain function. Many Nepali patients report:
- Forgetfulness
- Reduced productivity
- Slow thinking
- Difficulty focusing on tasks
Morning Headaches
These occur due to overnight oxygen drops and carbon dioxide buildup.
Irritability or Mood Changes
Family members often notice behavioral changes such as:
- Short temper
- Increased stress
- Mood swings
- Feeling demotivated
Sleep apnea affects emotional regulation.
Low Energy & Fatigue
Even light tasks can feel exhausting. People describe:
- “Heaviness”
- “Low battery feeling”
- No motivation in the morning
This is one of the most disabling symptoms for working individuals.
2.3 Symptoms Specific to Nepali Context
Nepal’s environment and lifestyle influence how sleep apnea presents.
Nasal Blockage & Sinus Issues
Dust, pollution, and allergies are common in Kathmandu, Pokhara, Butwal, and other urban centers. Blocked noses worsen sleep apnea symptoms and snoring.
Symptoms Mistaken for Gastric Problems
Many Nepali patients mistakenly think their fatigue or chest tightness is due to “gastric.”
In reality, untreated sleep apnea can also cause:
- Chest pressure
- Burning sensation
- Difficulty breathing at night
This leads to delayed diagnosis.
Dry, Tired Eyes in the Morning
Frequent micro-awakenings cause poor REM sleep → resulting in:
- Puffy eyes
- Eye strain
- Burning sensation
Often confused with screen fatigue.
2.4 Symptoms in Women (Often Different)
Women in Nepal often present symptoms that are less “classic” and more subtle:
- Insomnia instead of snoring
- Morning nausea
- Anxiety or depression
- Low stamina
- Headaches
- Restless sleep
Because these differ from men’s symptoms, many cases remain undiagnosed.
2.5 Symptoms in Older Adults
Elderly patients often do not report snoring but experience:
- Confusion or memory issues
- Frequent nighttime urination
- Morning dizziness
- Increased fall risk
Many families mistake these for “old age,” delaying testing.
2.6 Symptoms in Children
Children show different signs than adults:
- Mouth breathing
- Snoring
- Hyperactivity (not sleepiness)
- Bedwetting
- Poor school performance
- Behavioral issues
This is covered in detail in the pediatric chapter.
2.7 When Symptoms Get Worse
Symptoms often become severe when the patient:
- Gains weight
- Sleeps on the back
- Drinks alcohol
- Is under intense stress
- Has untreated allergies
- Uses sedative medications
2.8 When to Seek a Sleep Apnea Test
You should consider a sleep test if you notice:
- Loud, habitual snoring
- Daytime tiredness
- Morning headaches
- Observed breathing pauses
- Declining work performance
- Poor memory
- Mood swings
- High blood pressure
The earlier sleep apnea is diagnosed, the easier it is to treat.
CHAPTER 3 Types of Sleep Apnea Tests Available in Nepal
Diagnosing sleep apnea requires measuring how a person breathes, sleeps, and maintains oxygen levels throughout the night. In Nepal, two primary testing methods are available: a full overnight sleep study performed in a clinical setting and a home sleep apnea test done in the comfort of your own bedroom. Each test serves a different purpose and is recommended based on symptoms, lifestyle, and medical conditions.
This chapter explains the available test types clearly, without any overlap with symptoms or pricing sections.

3.1 Polysomnography (PSG) – Full Overnight Sleep Study
Polysomnography is the most comprehensive and medically detailed sleep test available in Nepal. It is performed in a dedicated sleep lab or hospital room under the supervision of trained sleep technicians.
This test uses multiple sensors to track how your body functions throughout the night.
What PSG Measures
Unlike basic tests, PSG monitors a wide range of parameters:
- Brain activity (EEG) – identifies sleep stages and disruptions
- Muscle tone (EMG) – detects limb movements, bruxism
- Eye movements (EOG) – tracks REM and non-REM cycles
- Oxygen saturation (SpO₂) – evaluates oxygen drops
- Airflow through nose and mouth
- Breathing effort (chest & abdomen belts)
- Heart rhythm (ECG)
- Snoring intensity
- Body position
These measurements form a complete picture of breathing-related sleep disturbances.
Why PSG Is Recommended
PSG is ideal when:
- Symptoms are severe or unclear
- Central sleep apnea is suspected
- Previous tests were inconclusive
- The patient has heart/neurological disorders
- There is concern about periodic leg movements, REM behavior disorder, or other sleep disorders
It is the gold standard for diagnosis worldwide.
3.2 Home Sleep Apnea Test (HSAT)
A Home Sleep Apnea Test is a simplified, portable test performed in your own bed, without the need to sleep in a clinic.
Compared to PSG, it uses fewer sensors and focuses mainly on breathing patterns.
What HSAT Measures
Depending on the device type, HSAT usually records:
- Airflow
- Breathing effort
- Oxygen saturation
- Heart rate
- Snoring
- Sleep position
HSAT is designed for detecting obstructive sleep apnea (OSA) — the most common type found in Nepal.
Why HSAT Is Recommended
HSAT is suitable when:
- Symptoms strongly indicate obstructive sleep apnea
- The patient wants a comfortable, at-home experience
- Quick diagnosis is needed
- Cost is a consideration
- There are no major heart or neurological conditions
This makes HSAT a highly convenient option, especially in urban areas like Kathmandu, Lalitpur, and Pokhara.
3.3 Levels of Sleep Testing (International Standard Classification)
Many people don’t know that sleep tests are categorized into different “types” or “levels.” This helps explain why some tests are more detailed than others.
Type I Sleep Test
- In-lab polysomnography (PSG)
- Supervised by a technician
- Most complete test (used in hospitals)
Type II Sleep Test
- At-home equipment but records nearly as many channels as PSG
- Less common in Nepal
Type III Sleep Test
- Standard Home Sleep Apnea Test (HSAT)
- Records 4–7 physiological signals
- Widely offered in Nepal
Type IV Sleep Test
- Simple airflow or oxygen sensors
- Not recommended for diagnostic accuracy
- Should be avoided for medical diagnosis
This classification helps patients understand what they are receiving — and why some tests offer deeper insights.
3.4 How Nepal Compares to Global Sleep Study Standards
Nepal’s major hospitals and private sleep centers now offer testing equipment similar to those used in international sleep labs.
- PSG (Type I) is available mainly in large hospitals and specialized centers.
- HSAT (Type III) is becoming widely available in Kathmandu and major cities.
- Ultra-basic tests (Type IV) still exist but are not recommended for diagnostic purposes.
Nepal’s testing quality has significantly improved in recent years due to better equipment, increased awareness, and wider availability of sleep specialists.
3.5 Choosing the Right Test for Your Symptoms
Choose PSG if you:
- Suspect central sleep apnea
- Have severe snoring + gasping
- Have heart disease, stroke history, or neurological disorders
- Had an inconclusive home test
- Experience limb movements, sleepwalking, or unusual behaviors at night
Choose HSAT if you:
- Have classic obstructive sleep apnea symptoms
- Want the comfort of sleeping at home
- Need a cost-effective, accurate screening
- Prefer a simpler, quicker process
- Do not have major comorbidities
Your doctor or sleep specialist will help determine which test fits your condition best.
CHAPTER 4 Sleep Apnea Test Costs in Nepal — A Complete Guide
The cost of a sleep apnea test in Nepal varies depending on the type of test, the technology used, and whether the test is performed at home or in a clinical sleep lab. While prices differ between facilities, the range is generally consistent across major cities, especially Kathmandu, where most sleep centers are located.
This chapter provides a clear, updated, non-repetitive cost breakdown so patients can confidently plan their testing journey.
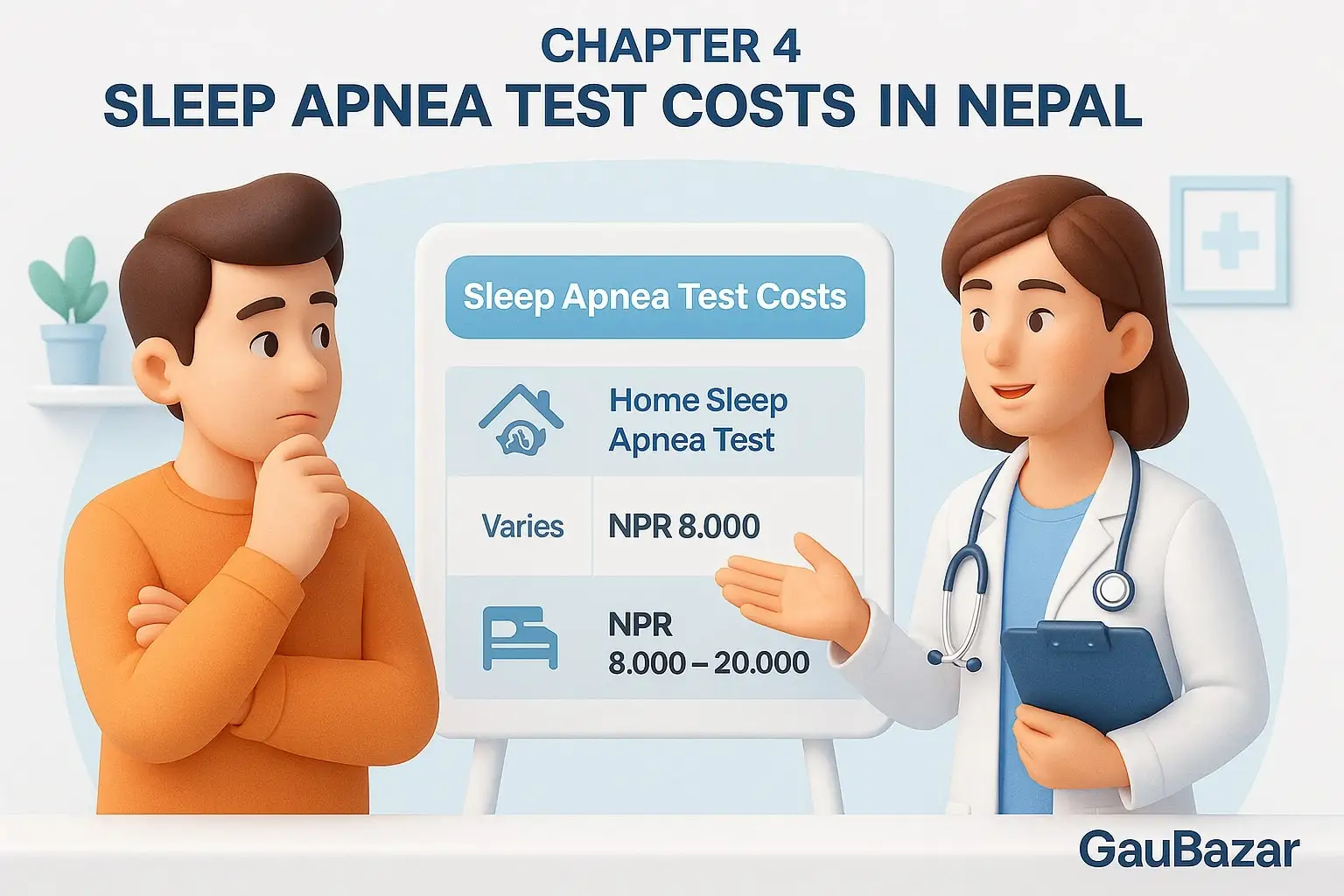
4.1 Cost of Home Sleep Apnea Test (HSAT)
Home Sleep Apnea Tests are typically the more affordable option. The cost depends on:
- Device quality
- Parameters measured
- Whether a sleep specialist interprets the results
- Follow-up consultation
HSAT is popular because it is simple, comfortable, and done at home, making it ideal for people with typical obstructive sleep apnea symptoms.
4.2 Cost of Polysomnography (Full Overnight Sleep Study)
A full in-clinic sleep study (Polysomnography or PSG) is the most detailed and medically comprehensive test available. It monitors multiple body functions, which makes it more resource-intensive.
Typical Price Range in Nepal (including Kathmandu):
NPR 8,000 – NPR 20,000
Price variation may depend on:
- Number of monitoring parameters
- Sleep lab setup (standard vs. private room)
- Equipment sophistication
- Technician involvement
- Reporting depth
- Option for CPAP/BiPAP trial during study
Even though the cost is higher than HSAT, PSG is the gold standard for diagnosing complex sleep disorders.
4.3 Pricing Table
Test Type | Typical Price (NPR) | What’s Included | Best For |
|---|---|---|---|
Home Sleep Apnea Test (HSAT) | Varies by clinic | Portable device, monitoring, basic interpretation | Mild–moderate symptoms, convenience |
Polysomnography (PSG) | Rs. 8,000 – 20,000 | Full overnight study, technician support, detailed report | Complex, severe, or unclear cases |
4.4 Why Sleep Test Prices Vary Across Nepal
Prices differ for several reasons:
- Quality of sensors and monitoring devices
- Experience of sleep technicians
- Depth of report interpretation
- Additional follow-up or treatment guidance
- Facility type (hospital vs. private clinic)
Higher prices don’t always mean better care, but extremely low prices may mean fewer monitored parameters or limited support.
4.5 Testing in Kathmandu: What Patients Should Expect
Kathmandu offers the widest range of sleep testing facilities and most advanced equipment in the country. While prices generally fall within the national range, Kathmandu centers often provide:
- Faster appointment availability
- Superior equipment quality
- Trained sleep technologists
- Optional CPAP/BiPAP titration
- Comfortable sleep lab environments
For many patients around Nepal, Kathmandu remains the preferred location for a full sleep study.
CHAPTER 5 Sleep Test Accuracy — What Patients Should Know
A sleep apnea test is only useful when it provides accurate, reliable, and clinically meaningful results. In Nepal, patients often wonder whether they should choose a home sleep test or a full overnight sleep study — and whether both tests are truly dependable. This chapter explains how accurate each test is, what accuracy means medically, and when results can be trusted or questioned.
5.1 What Accuracy Means in Sleep Testing
Accuracy in a sleep apnea test refers to how precisely the test can measure:
- Breathing disturbances
- Oxygen drops
- Sleep disruptions
- Snoring patterns
- Heart-related changes
These measurements help doctors determine the severity, type, and pattern of sleep apnea — all essential for a proper treatment plan.
5.2 Accuracy of Polysomnography (PSG)
Polysomnography, performed in a controlled clinical environment, is the gold standard worldwide for diagnosing sleep apnea.
Why PSG Is Highly Accurate
- Measures the highest number of physiological signals
- Tracks brain activity (crucial for identifying real sleep time)
- Detects subtle breathing irregularities
- Identifies central sleep apnea
- Captures limb movements and sleep behavior issues
- Provides precise AHI (Apnea-Hypopnea Index) calculation
PSG accuracy is the most reliable for diagnosing any type of sleep apnea and is especially recommended for:
- Severe symptoms
- Complex breathing patterns
- Patients with heart or neurological conditions
- Cases where home tests are inconclusive
PSG results are typically 95–98% accurate when performed correctly.
5.3 Accuracy of Home Sleep Apnea Tests (HSAT)
Home Sleep Apnea Tests are designed to diagnose obstructive sleep apnea (OSA) in adults who have clear symptoms.
When HSAT Is Highly Accurate
- Patient has typical OSA symptoms
- No major medical conditions
- Device is worn properly all night
- Minimum of 4 hours of good-quality data
- Snoring and breathing patterns are straightforward
HSAT focuses on breathing-related signals rather than full sleep stages, but for common OSA cases, accuracy is high.
Limitations (Important)
HSAT may be less accurate if:
- The patient frequently wakes up
- The device shifts during sleep
- The person has central or mixed apnea
- There are neurological, cardiac, or chronic respiratory conditions
- The patient sleeps very little during the test
HSAT accuracy is generally 80–90% for typical obstructive sleep apnea.
5.4 When a Home Test May Miss Sleep Apnea
Because HSAT measures fewer parameters, it may underestimate or miss apnea in certain situations. This is called a false negative.
HSAT may miss apnea if:
- Apnea only occurs during REM sleep
- Symptoms are mild
- Apnea occurs only when sleeping on the back
- The patient has short sleep duration
- Oxygen drops are minimal
- The person has periodic limb movements or parasomnias
In these cases, doctors often recommend a follow-up PSG.
5.5 Understanding Sensitivity and Specificity (Simple Explanation)
Doctors use two concepts to evaluate test accuracy:
Sensitivity
How well the test identifies people who HAVE sleep apnea.
High sensitivity = fewer missed diagnoses.
Specificity
How well the test identifies people who DO NOT have sleep apnea.
High specificity = fewer false alarms.
- PSG has both high sensitivity and specificity.
- HSAT has good specificity but lower sensitivity, which means it may miss mild cases.
5.6 When Doctors Recommend a Repeat Test
A sleep specialist may order a second test if:
- Results don’t match your reported symptoms
- The test collected less than 4 hours of usable data
- You continued to remove sensors unknowingly
- Technical issues occurred
- Your condition worsens over time
- Initial results were borderline or unclear
Repeat testing is common and ensures the diagnosis is fully accurate.
5.7 Why Accuracy Matters for Treatment
Accurate sleep test results help determine:
- Correct AHI severity (mild, moderate, severe)
- Whether CPAP, BiPAP, or APAP is required
- What pressure settings should be used
- Whether surgery or oral appliances may help
- If the apnea is obstructive, central, or mixed
- Whether additional tests are needed
Poor accuracy may lead to wrong treatment, ineffective therapy, or worsening symptoms.
5.8 How to Improve Test Accuracy (Patient Tips)
You can improve your test’s accuracy by:
- Wearing sensors tightly but comfortably
- Avoiding caffeine or alcohol before bedtime
- Keeping your sleep schedule normal
- Sleeping in your usual position
- Ensuring the device battery is full
- Following technician instructions precisely
- Not removing sensors during sleep
These small steps significantly enhance the clarity of the recorded data.
CHAPTER 6 What to Expect During a Sleep Apnea Test
Most patients feel nervous before their first sleep apnea test simply because they don’t know what to expect. In reality, the process is comfortable, simple, and designed to monitor your natural sleep as closely as possible.
This chapter explains the entire experience — step by step — so you feel confident and prepared.
We cover both Polysomnography (PSG) done in a clinic and Home Sleep Apnea Tests (HSAT) done at home.
6.1 Before the Test: How to Prepare (Simple & Patient-Friendly)
Your preparation impacts the quality of your sleep data. Clinics in Nepal usually recommend:
- Follow your normal routine: Maintain your usual sleep schedule to help the device capture natural patterns.
- Avoid alcohol & caffeine: Both can alter your breathing and sleep cycles.
- Do not use lotions or oils on the skin: Sensors attach more effectively on clean, dry skin.
- Bring your medication list: Some medicines influence sleep and breathing, so the technician must be informed.
- Wear comfortable, loose clothing: Choose a T-shirt and shorts or pajamas.
- Eat a light dinner: Avoid heavy meals before bedtime.
This preparation helps ensure a smooth testing experience.
6.2 What Happens During an Overnight Polysomnography (PSG)
If you take the full sleep study at a clinic or hospital, this is what you will experience.
Arrival & Check-In
You arrive in the evening — usually between 7 PM to 9 PM.
A sleep technician welcomes you and guides you to a private room designed for comfort, not a “hospital-like” environment.
Sensor Setup (Non-Painful & Quick)
The technician attaches several small sensors to your:
- Scalp
- Chin
- Chest
- Legs
- Around your nose
- Near your abdomen
These sensors do not hurt — they are held in place with medical tape or soft adhesive gel. You can move, change positions, and sleep as you normally do.
Airflow & Breathing Monitoring
A soft nasal cannula or airway sensor is placed to monitor airflow.
This is light and comfortable.
Sleeping Normally
Once you’re ready:
- Lights are turned off
- The technician monitors data from another room
- You can roll, turn, and sleep on your side or back
- You can get up to use the bathroom anytime
- You are not “watched” visually unless required
The goal is to capture your natural sleep, not force you into a restricted environment.
Overnight Monitoring
Throughout the night, the system records:
- Breathing patterns
- Oxygen changes
- Sleep stages
- Heart rhythm
- Snoring levels
- Body movements
If a sensor detaches while you sleep, the technician may gently reattach it.
Morning Wake-Up
You wake up early — around 5 AM to 6 AM — and the technician removes all sensors.
You can leave immediately and continue your normal day.
6.3 What Happens During a Home Sleep Apnea Test (HSAT)
Home tests are simpler, comfortable, and done in your own bedroom.
Device Pickup or Technician Visit
Depending on the clinic:
- A technician may visit your home
- You may collect the device from the center with guidance
Self-Applying the Sensors
You are shown how to attach:
- Airflow sensor (under the nose)
- Breathing effort belts (chest and abdomen)
- Finger oximeter (for oxygen levels)
- Small recorder unit (device box)
These sensors are fewer and simpler than a full PSG.
Sleeping Naturally in Your Own Bed
You sleep at home — in your familiar environment — which often gives natural data.
You don’t need video monitoring or a technician present.
Returning the Device
The next morning:
- You remove the sensors
- Return the device to the clinic
- A technician downloads and analyzes your data
6.4 Comfort & Safety During the Test
- Sensors are painless and safe: All leads are designed for comfort, with no needles or invasive attachments.
- You can sleep in any position: Except when the provider advises otherwise for specific reasons.
- No electric shocks or risk: All equipment operates on low-voltage medical systems.
- Full privacy: You sleep alone; technicians monitor data only, not your personal space.
6.5 What You Will NOT Experience (Myth-Busting)
Patients often fear things that don’t happen:
❌ You will NOT be shocked by wires
❌ You will NOT be forced to sleep in one position
❌ You will NOT be watched directly all night
❌ You will NOT feel pain
❌ You will NOT be attached to heavy machines
❌ You will NOT be exposed to radiation
Sleep tests are extremely safe and non-invasive.
6.6 After the Test: What Happens Next
Data Analysis
Technicians score your breathing events, oxygen fluctuations, and sleep disruptions.
Specialist Interpretation
A sleep specialist reviews the results and prepares your detailed report.
Diagnosis & Treatment Options
Depending on the severity, you may be advised:
- CPAP, APAP, or BiPAP therapy
- Lifestyle changes
- Oral appliances
- Surgery (in select cases)
Your doctor will explain the results clearly and help you choose the right treatment.
CHAPTER 7 Understanding Your AHI Score
When a sleep study is finished you’ll receive a formal report. The most important number people notice first is the AHI — the Apnea–Hypopnea Index — but the report contains several related measures that together explain what is happening during your sleep. This chapter explains those numbers in plain language, how clinicians interpret them, and what actions follow different results.
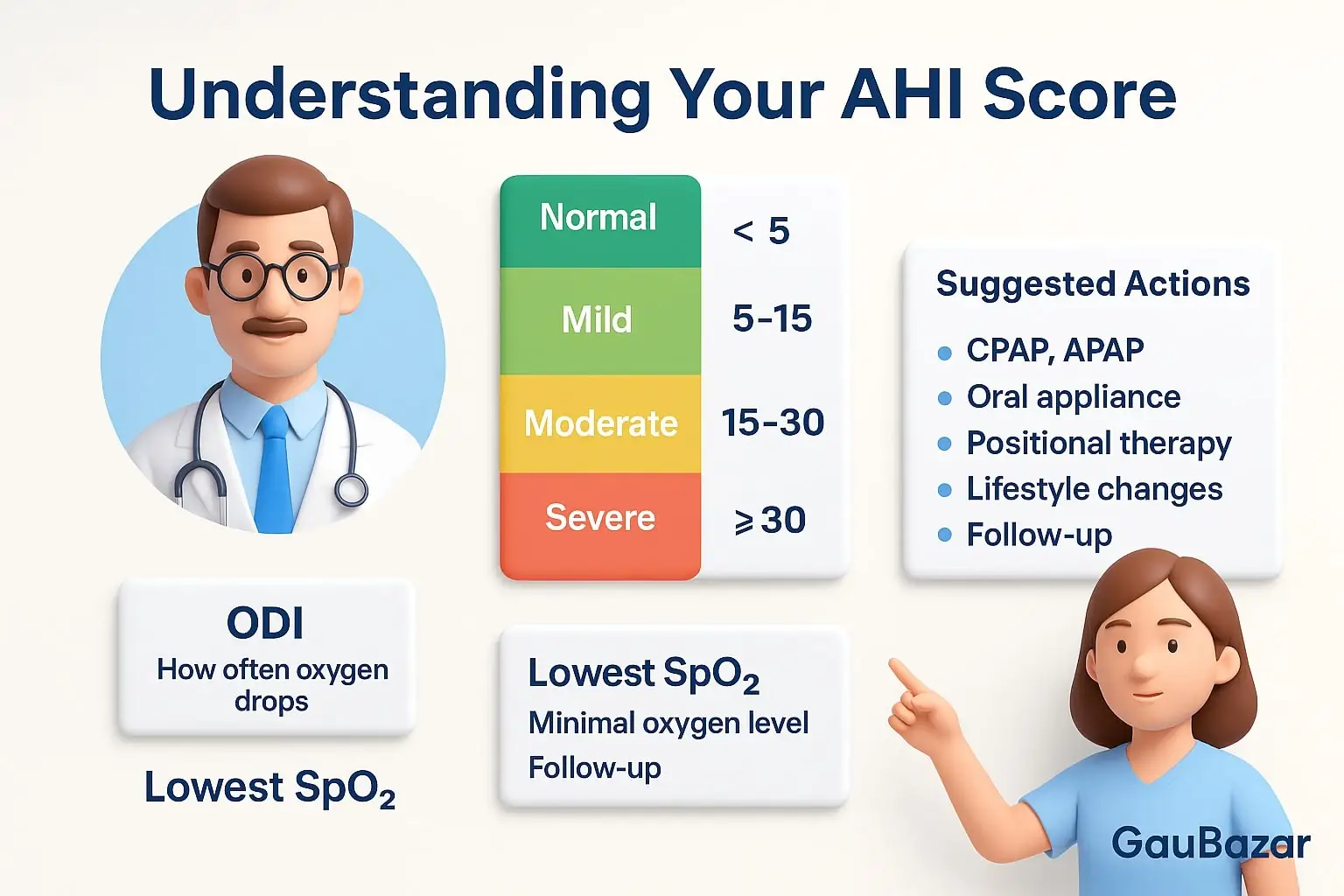
7.1 Key terms made simple
- Apnea — a complete pause in breathing for at least a few seconds.
- Hypopnea — a partial reduction in airflow that is large enough to cause oxygen drop or sleep disruption.
- AHI (Apnea–Hypopnea Index) — the average number of apneas + hypopneas per hour of sleep. This is the headline measure of severity.
- ODI (Oxygen Desaturation Index) — the number of times per hour the blood oxygen level falls by a preset amount (commonly ≥3–4%). ODI shows how often breathing events cause significant oxygen drops.
- RDI (Respiratory Disturbance Index) — like AHI but can include other respiratory events (arousals without clear hypopnea). Some labs report RDI instead of AHI.
- Lowest SpO₂ / Mean SpO₂ — the lowest recorded oxygen saturation and the night’s average saturation; these indicate how low and how sustained oxygen drops were.
- Sleep Time vs. Recording Time — PSG measures true sleep time (time actually asleep); some home devices estimate sleep time from breathing signals. Knowing which is used affects how AHI is calculated.
7.2 How severity is classified (practical thresholds)
Clinicians categorize AHI to guide treatment decisions:
- AHI < 5 — normal/minimal
- AHI 5–15 — mild sleep apnea
- AHI 15–30 — moderate sleep apnea
- AHI > 30 — severe sleep apnea
Remember: these numbers are guides — treatment decisions also rely on symptoms, oxygen drops, cardiac risks, and daytime function.
7.3 Examples to make it concrete
- Someone with AHI 8 who is very sleepy and has heart failure may be treated more aggressively than a symptom-free person with the same AHI.
- A patient with AHI 28 and repeated dips below 85% oxygen will usually be offered therapy promptly.
- A home test that reports an AHI of 4 but shows frequent brief desaturations or very fragmented sleep may still prompt a full lab study.
7.4 Important nuances clinicians look for (why numbers alone are not enough)
- When and where events occur: REM-related apnea (events concentrated in REM sleep) or supine-only apnea (worse on the back) may change therapy choices (positional therapy, REM-targeted strategies).
- Duration and depth of desaturations: Frequent shallow drops are different from fewer deep, prolonged drops — the latter carry higher cardiovascular risk.
- Arousal burden: Many brief arousals fragment sleep and cause daytime sleepiness even if AHI is moderate.
- Event morphology: Central events (lack of effort) indicate a different problem than obstructive events (airflow blocked despite effort).
- Total sleep time accuracy: In-lab PSG calculates AHI per real sleep time; some home tests estimate sleep time and may under- or over-estimate AHI.
7.5 How to read your report — practical checklist
When you receive the report, check these elements and discuss them with your clinician:
- AHI / RDI number — note the value and severity category.
- ODI and Lowest SpO₂ — are desaturations frequent and deep?
- Sleep architecture summary (PSG only) — how much deep and REM sleep did you get?
- Position/REM breakdown — are events concentrated in REM or supine position?
- Event types — obstructive vs central.
- Recommended conclusion — does the specialist recommend CPAP, oral appliance, positional therapy, or further testing?
Bring the report to your follow-up and ask for explanations of any unfamiliar terms.
7.6 Common questions patients ask (short answers)
- “Is AHI the only thing that matters?” No — symptoms and oxygen drops matter equally.
- “Can AHI change night to night?” Yes — sleep position, alcohol, nasal congestion, and sleep stage distribution can change AHI.
- “If my AHI is mild, do I still need treatment?” If you have significant daytime sleepiness, cardiovascular disease, or frequent oxygen drops, treatment is often recommended even for mild AHI.
- “What if my home test and PSG disagree?” A PSG is considered more reliable; your doctor may recommend PSG if clinical suspicion remains high.
7.7 When additional testing is needed
- Borderline or conflicting results (e.g., symptoms are severe but AHI is low) → repeat PSG or consider extended monitoring.
- Suspected central apnea → full PSG with CO₂ monitoring or cardiology/neuro evaluation.
- Large oxygen desaturations despite low event count → evaluate for lung disease or nocturnal hypoventilation.
7.8 Practical next steps after seeing your AHI
- If AHI is moderate-to-severe, expect a discussion about positive airway pressure (CPAP/APAP/BiPAP) and mask fitting.
- For positional or REM-limited apnea, discuss positional therapy or lifestyle measures.
- If AHI is mild and symptoms are minimal, start with lifestyle interventions and follow up.
- In all cases, schedule a follow-up to review how symptoms change after any intervention.
7.9 A short patient-friendly summary
AHI tells you how often your breathing is disrupted per hour, but the full story involves oxygen drops, when events occur, and how you feel during the day. Use your report as a map — the numbers guide treatment, but your doctor will tailor therapy based on the whole picture.
CHAPTER 8 Treatment Options After Diagnosis
Once your sleep test is completed, the next step is choosing the right treatment based on your test results, AHI pattern, oxygen levels, symptoms, age, and underlying health conditions. Treatment is personalized — no single therapy works for everyone. The goal is simple: keep the airway open, normalize oxygen levels, and help you sleep deeper and safer.
Below are the most effective, medically recognized treatment options available in Nepal.
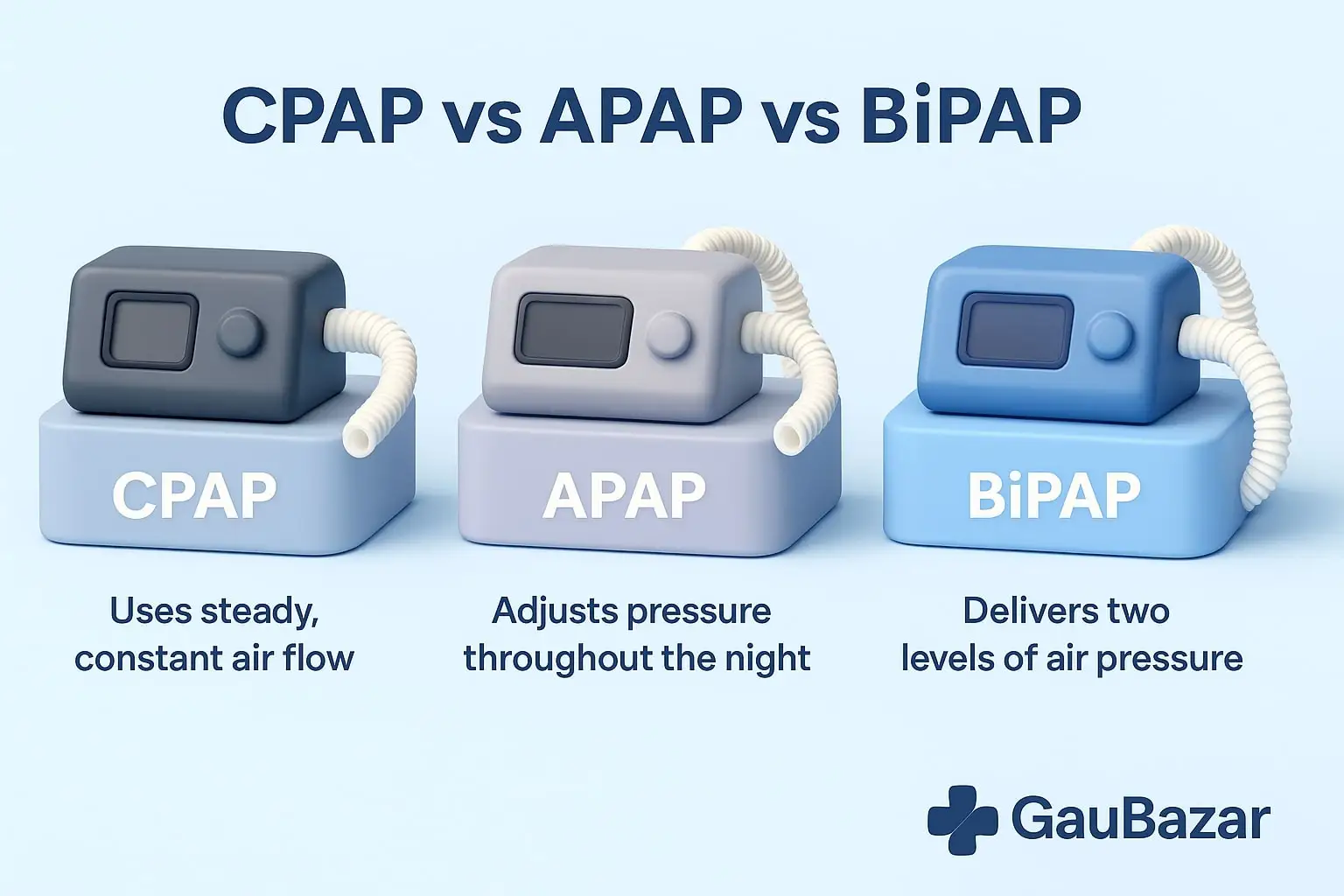
8.1 CPAP Therapy (Continuous Positive Airway Pressure)
CPAP is the first-line treatment for moderate to severe obstructive sleep apnea (OSA).
It provides a steady, constant airflow that keeps your airway open so you breathe normally throughout the night.
Benefits of CPAP:
- Eliminates snoring and gasping
- Restores deep sleep
- Improves daytime energy
- Reduces morning headaches
- Lowers blood pressure
- Protects heart & brain health
- Improves focus and productivity
Who should use CPAP?
- Moderate or severe OSA
- People with oxygen drops during the night
- Patients with loud snoring + choking
- Those with hypertension or heart issues
- CPAP is highly effective when used consistently.
8.2 APAP Therapy (Auto-Adjusting Positive Airway Pressure)
APAP automatically adjusts the air pressure depending on how your breathing changes throughout the night.
Why people prefer APAP:
- More comfortable than fixed pressure
- Adapts to changes in sleep position
- Great for beginners
- Ideal for mild to moderate OSA
- Reduces the need for manual pressure adjustments
APAP is widely used because of its comfort and adaptability.
8.3 BiPAP Therapy (Bilevel Positive Airway Pressure)
BiPAP delivers two levels of airflow:
- Higher pressure when you inhale (IPAP)
- Lower pressure when you exhale (EPAP)
BiPAP is recommended for:
- People who cannot tolerate CPAP
- Those needing higher pressure support
- Patients with central sleep apnea
- People with COPD or neuromuscular disorders
- Obesity hypoventilation syndrome
- People who retain CO₂
BiPAP is particularly helpful for complex cases that need extra breathing support.
8.4 Oral Appliance Therapy (Mandibular Advancement Devices)
These are custom-made dental devices that gently hold the lower jaw forward, preventing the airway from collapsing.
Best for:
- Mild to moderate obstructive sleep apnea
- People who cannot tolerate CPAP/APAP
- Frequent travelers
- Snoring-focused cases
These devices are compact, comfortable, and effective when fitted properly.
8.5 Positional Therapy
Some patients experience apnea only when sleeping on their back (supine position).
This is called positional sleep apnea.
Treatment tools include:
- Positional belts
- Special pillows
- Small vibrating devices that alert you when you roll onto your back
Positional therapy is simple but surprisingly effective for the right patient type.
8.6 Lifestyle Therapy
Lifestyle changes cannot “cure” sleep apnea alone, but they significantly improve symptoms and long-term health.
Helpful adjustments include:
- Weight management
- Avoiding alcohol 3–4 hours before bedtime
- Treating nasal allergies
- Following a regular sleep schedule
- Exercising regularly
- Reducing smoking
- Improving diet quality
When combined with medical therapy, lifestyle changes enhance treatment success.
8.7 Nasal & Airway Support
For people with chronic nasal congestion — a common issue in Nepal due to dust and pollution — clearing the airway can improve nightly breathing.
Helpful options:
- Antiallergy treatment
- Nasal sprays
- Saline rinses
- Steam inhalation
- Treating sinus infections
A clear nasal passage increases CPAP comfort and reduces snoring.
8.8 Surgical Options
Surgery is considered only when other therapies fail or when a clear structural blockage exists.
Common surgeries include:
- UPPP – removes excess tissue in the throat
- Septoplasty – corrects deviated septum
- Turbinate reduction – improves nasal airflow
- Tonsillectomy/adenoidectomy – especially effective in children
- Maxillomandibular advancement (MMA) – moves jaw forward to expand airway
- Hypoglossal nerve stimulation – advanced treatment for selected patients
Surgery is not the first option for most adults but can be highly beneficial in specific cases.
8.9 Treatment for Central Sleep Apnea
This condition requires different management compared to obstructive apnea.
Treatments include:
- Adaptive servo-ventilation (ASV)
- BiPAP with backup rate
- Treating underlying heart or neurological conditions
- Medication adjustments
Central apnea must be treated by a specialist.
8.10 Pediatric Sleep Apnea Treatment
Children often have airway obstruction caused by enlarged adenoids or tonsils.
Common solutions:
- Adenoidectomy
- Tonsillectomy
- Allergy management
- Orthodontic therapy for jaw alignment
- Weight management (if applicable)
Children respond well to early treatment.
8.11 When Follow-Up Is Necessary
Follow-up is essential to ensure your treatment is working.
Your doctor may recommend:
- A repeat sleep test
- CPAP pressure adjustment
- Mask refitting
- Review of daytime symptoms
- Monitoring oxygen levels
Sleep apnea treatment improves quickly with proper follow-up.
CHAPTER 9 Who Should Get Tested in Nepal?
Sleep apnea often goes undiagnosed in Nepal because many people assume tiredness, snoring, or poor sleep is “normal.” A sleep apnea test becomes important when certain patterns, medical conditions, or lifestyle factors suggest that your breathing may be disrupted at night.
This chapter explains who should get tested, based on clinical guidelines and practical considerations specific to Nepali patients—without repeating earlier content.

9.1 People With Sleep-Related Red Flags
A sleep test is recommended when nighttime breathing concerns are suspected, especially if:
- Someone observes unusual breathing during your sleep
- You frequently wake up feeling unrefreshed despite full sleep
- Your sleep seems fragmented without an obvious cause
These patterns suggest your sleep quality is being disturbed by breathing irregularities.
9.2 Individuals Experiencing Persistent Daytime Dysfunction
If your daily functioning is affected in ways you cannot explain, a sleep study may help identify underlying nighttime breathing issues.
You should test if you experience any combination of:
- Reduced alertness during routine tasks
- Difficulty staying awake during passive activities
- Slower decision-making
- Reduced productivity or mental clarity
- Unusual irritability or mood swings
These signs indicate that your sleep may not be restorative, even if you think you’re sleeping long enough.
9.3 People With Medical Conditions That Often Hide Sleep Apnea
Certain health issues make sleep apnea more likely, even if symptoms are mild. You should get tested if you have:
Cardiovascular concerns
- Uncontrolled blood pressure
- Irregular heartbeat
- History of stroke
- Congestive heart problems
Metabolic conditions
- Type 2 diabetes
- Insulin resistance
- Obesity or rapid weight gain
Respiratory or airway issues
- Chronic nasal blockage
- Allergic rhinitis (common in Nepal due to pollution)
- Long-term sinus difficulties
When these conditions coexist with poor sleep quality, a sleep test becomes essential.
9.4 People Whose Jobs Require High Alertness
Some professions cannot risk reduced concentration, micro-sleep, or delayed reactions.
Testing is strongly recommended for:
- Bus / truck / taxi drivers
- Delivery and logistics operators
- Factory machine operators
- Security personnel
- Medical professionals
- Aviation and technical staff
- Night-shift and rotating-shift workers
Even mild sleep-disruption patterns can be dangerous in these roles.
9.5 Men and Women Over 40
After age 40, natural changes in airway structure, muscle tone, and sleep regulation increase vulnerability to breathing-related sleep issues. Men have a higher risk earlier, but women’s risk rises sharply after menopause.
Testing is recommended if you notice:
- Gradual decline in morning freshness
- Increasing fatigue over months
- Sudden change in sleep stability
Even small changes in nighttime breathing can accumulate and affect long-term health.
9.6 People Living in High-Pollution or High-Allergy Zones in Nepal
Nepal’s environmental conditions contribute significantly to nighttime breathing problems.
Testing is recommended for people living in:
- Kathmandu Valley (dust, smog, construction pollution)
- Industrial cities like Birgunj, Bhairahawa, Nepalgunj
- Areas with seasonal fires or heavy allergens
Long-term exposure leads to persistent inflammation of the airway, which increases the likelihood of sleep-related breathing disruptions.
9.7 Individuals Who Feel “Something Is Wrong” With Their Sleep
Many Nepali patients report a consistent pattern of vague, hard-to-explain sleep discomfort before being diagnosed.
You should consider testing if you experience:
- A sense of “unfinished sleep”
- Difficulty waking up despite long sleep
- Feeling mentally dull in the morning
- Frequent awakenings without clear reason
- Occasional episodes of “waking up suddenly”
These subtle experiences are often early indicators of breathing instability during sleep.
9.8 When an Immediate Test Is Recommended
Testing should not be delayed if you:
- Have had near-falls-asleep while driving
- Experience sudden awakenings with discomfort
- Have significantly decreasing energy levels
- Notice changes in memory or decision-making
- Recently had a heart or neurological event
These scenarios may indicate moderate or severe sleep disruption and deserve prompt evaluation.
9.9 Summary: Should YOU Get Tested?
You should get a sleep apnea test in Nepal if:
- Your sleep does not feel refreshing
- Others notice unusual nighttime breathing
- You struggle with unexplained daytime tiredness
- You have underlying medical risks
- You work in a profession requiring alertness
- You live in areas with poor air quality
- You feel concerned about any change in sleep quality
Testing is simple, affordable, and can prevent long-term complications.
CHAPTER 10 How to Choose a Sleep Testing Center in Nepal
Selecting the right sleep testing center is crucial for getting a correct diagnosis and a reliable treatment plan. Not all sleep labs or clinics in Nepal maintain the same standards, equipment quality, or level of expertise. The right center ensures you receive accurate evaluation, professional support, and clear guidance from start to finish.
Below is a practical guide to help you choose a dependable, high-quality sleep testing center in Nepal — without repeating any information from earlier chapters.
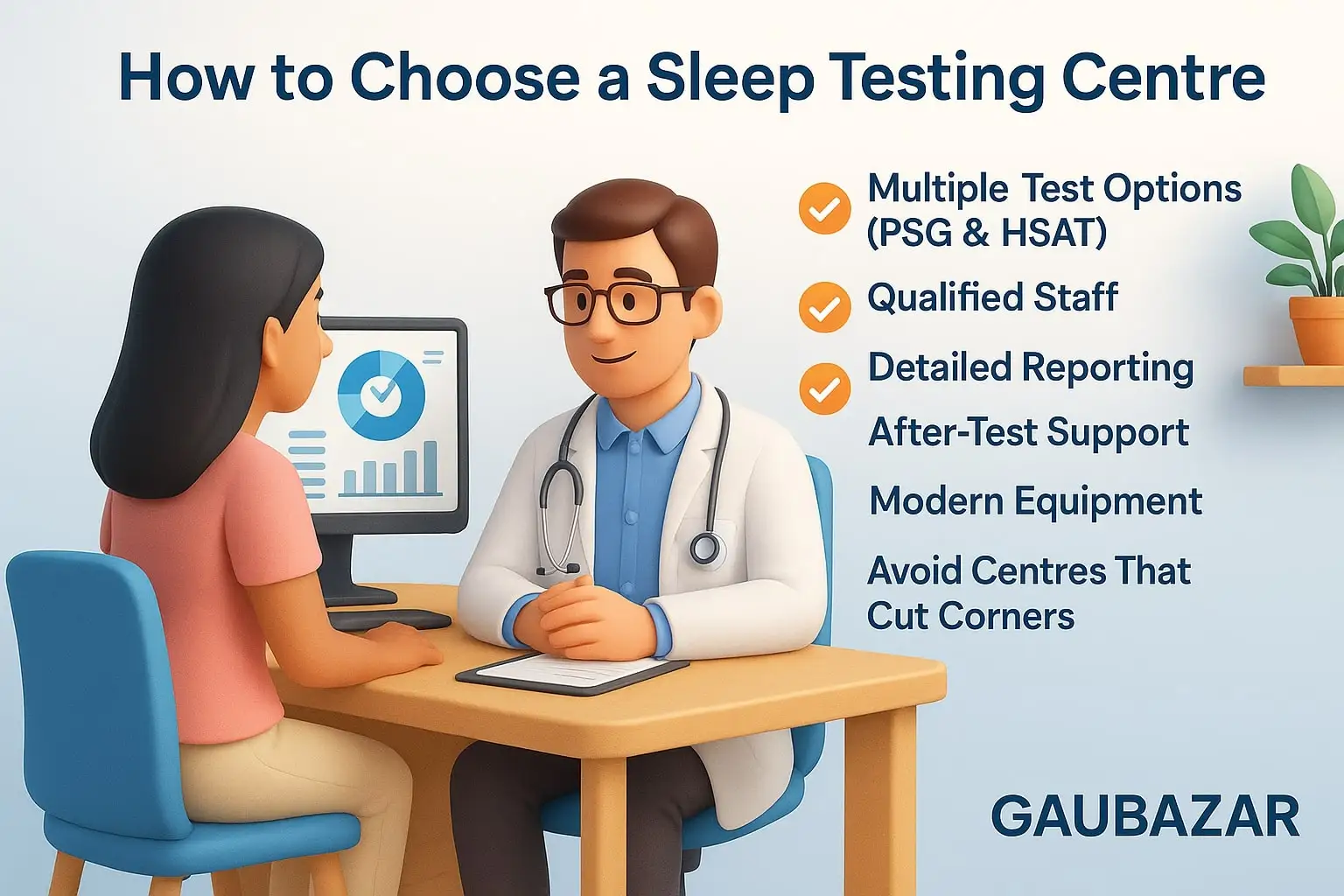
10.1 Look for Centers That Offer More Than One Testing Method
A credible centre should offer multiple testing options rather than pushing every patient toward a single method. This shows they understand that each case requires individualized evaluation.
A good center typically offers:
- Full in-lab overnight study (PSG)
- Home-based sleep apnea test (HSAT)
Having both available ensures you’re recommended the test that fits your condition, not the clinic’s convenience.
10.2 Ask About the Qualification of the Staff
A professional sleep centre should have:
- Technicians trained in sleep study setup
- Staff who can troubleshoot sensors
- Sleep professionals who can analyze data
- Access to sleep physicians or pulmonologists
The competence of the staff directly affects recording quality, patient comfort, and accuracy of results.
10.3 Check Reporting Quality — Not Just the AHI Number
A high-quality sleep test report includes:
- Clear explanation of breathing patterns
- Oxygen trend charts
- Breakdown of sleep positions and their impact
- Separation of obstructive vs central events
- Actionable treatment recommendations
Centers that provide only a one-page summary or AHI number should be avoided.
A detailed report is essential for long-term treatment success.
10.4 Verify That Equipment Is Modern and Properly Maintained
Equipment quality makes a big difference. Look for centers that use:
- Certified medical-grade devices
- Updated software
- Properly calibrated sensors
- Clean, well-maintained accessories
Higher-end devices capture more accurate data and minimize test errors.
10.5 Make Sure the Centre Offers After-Test Support
A sleep test alone does not solve the problem — you need interpretation and guidance afterward.
Choose centers that provide:
- A follow-up consultation to explain results
- Guidance on treatment options
- Help with device selection (CPAP/APAP/BiPAP) if required
- Referral support for ENT or cardiac evaluation when needed
Centers that only hand over the report and end the process leave patients confused and untreated.
10.6 Check the Environment and Comfort Level (for PSG)
For overnight in-lab testing, the room should be:
- Quiet
- Clean
- Temperature-controlled
- Comfortable for sleeping
- Equipped with hygienic bedding
A peaceful environment ensures more natural sleep, which improves data quality.
10.7 Consider Turnaround Time for Reports
Good centers typically provide results within:
- 24–72 hours for HSAT
- 2–4 days for PSG
Long delays may indicate poor workflow or insufficient staff.
10.8 Look for Transparency and Clear Communication
A trustworthy sleep testing center will:
- Explain what the test measures
- Tell you what to expect
- Provide instructions for preparation
- Answer questions clearly
- Explain follow-up steps
Transparency builds trust and ensures you’re informed throughout the process.
10.9 Avoid Centers That Cut Corners
Be cautious about centers that:
- Offer extremely cheap tests with unclear equipment
- Don’t show their devices
- Don’t explain reporting details
- Don’t offer interpretation or follow-up
- Use outdated or single-sensor devices
- Push the same test type to everyone
A proper sleep test requires quality equipment + trained staff + thorough reporting.
10.10 Questions to Ask Before Choosing a Centre
Before booking, ask:
- What type(s) of sleep tests do you offer?
- Who analyzes the data?
- How detailed will my report be?
- Is a consultation included after the test?
- What equipment brand do you use?
- What support is provided if something goes wrong during the test?
- How soon will I receive the results?
Their answers will immediately reveal their professionalism.
FAQ SECTION
1. Is a sleep apnea test painful?
No. Both PSG and home sleep tests use external sensors placed on the skin. There are no needles, no injections, and no discomfort involved.
2. Is a home sleep test accurate enough?
Yes — for straightforward cases of suspected obstructive sleep apnea.
However, complex cases (central apnea, heart conditions, unclear symptoms) may require a full in-lab PSG for deeper analysis.
3. Does snoring always mean sleep apnea?
Not necessarily.
Snoring can occur without apnea, but habitual, loud, or disruptive snoring is one of the strongest early indicators that a person should be evaluated.
4. How often should I repeat a sleep test?
A repeat test is recommended when:
- Symptoms noticeably change
- You begin CPAP/APAP/BiPAP and need pressure reassessment
- You gain or lose significant weight
- Your doctor requests follow-up data
5. Can children undergo a sleep study?
Yes. Children can be evaluated using pediatric sleep testing protocols, which use child-friendly sensors and age-adjusted scoring criteria.
6. Do I need a doctor’s referral?
In most cases, no referral is required. Patients can directly book a sleep test, and the interpreting physician will guide next steps.
7. Will insurance cover the test in Nepal?
Coverage varies. Some private policies may reimburse part of the cost, but many patients pay directly. It’s best to check with your insurer before booking.
8. How long does it take to get results?
Most centers provide HSAT results within 24–72 hours and PSG results within 2–4 days, depending on analysis complexity.
Final Message
If you or someone close to you has been experiencing poor sleep, unexplained tiredness, loud snoring, or concerns about nighttime breathing, now is the right time to act.
A sleep apnea test is simple, safe, and one of the most effective ways to understand what is happening inside your body while you sleep.
Early diagnosis protects your heart, improves energy, sharpens your mind, and restores quality of life.

👉 Take the first step toward better sleep and better health today.
Testing early can prevent years of fatigue, frustration, and silent health risks.
Buy CPAP & BiPAP Machines in Nepal
